UnitedHealthcare health plans do not cover COVID-19 surveillance testing, which is testing used for public health or social purposes such as employment (return to workplace), education, travel or entertainment. Medicare also covers COVID-19 antibody test s, COVID-19 monoclonal antibody . Care providers can connect to the latestCenters for Disease Control and Prevention (CDC)guidance for health professionals, as well astravel advisories from the U.S. State Department. The information provided through this service is for informational purposes only. If you don't find the provider you are searching for, you may contact the provider directly to verify participation status with UnitedHealthcare's network, or contact Customer Care at the toll-free number shown on your UnitedHealthcare ID card. Thankfully, there is no longer a supply shortage. Some service or facility exclusions may apply. 0 Both therapies should only be prescribed by physicians, advanced practice registered nurses and physician assistants that are licensed or authorized under state law to prescribe drugs in the anti-infective class. Coding, Submissions & Reimbursement | UHCprovider.com Centers for Medicare and Medicaid Services. We do not guarantee that each provider is still accepting new members. endobj What Happens When COVID-19 Emergency Declarations End - KFF Individuals appropriate for treatment are those with a positive COVID-19 viral test result and who are at high risk for progression to severe COVID-19, including hospitalization or death. Typical processes and member benefits, including those related to clinical trial participation, if applicable, will apply for outpatient visits. Limitations, co-payments, and restrictions may apply. Sign in to your online UnitedHealthcare account or review your plan materials for details on your benefit plan. This includes employer-sponsored health plans as well as individual/family health plans that people purchase themselves (including grandmothered and grandfathered plans). Updated February 2, 2023|7:30 AM CST, Download virtual visits and telehealth FAQs For UnitedHealthcare Community Plan members, coverage of COVID-19 testing is determined by each State Medicaid program, and specifics regarding coverage vary by state. UnitedHealthcare's Coronavirus (COVID-19) Home Page. UnitedHealthcare Connected for MyCare Ohio (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. The guidelines ensure that health plans cover the cost of COVID tests regardless of any other factors; a person does not have to be symptomatic or under a doctor's care, and can simply obtain the tests over the counter at a pharmacy. Virtual visits, also called telehealth, gives you access to health care providers from the comfort of your home. Updated April 21, 2023|7:50 PM CST, Download treatment and coverage FAQs "Nothing has changed in the claims-paying process as a result of COVID-19 vaccinations.". Part A, Part B, and supplemental Part C plan benefits are to be provided at specified non- contracted facilities (note that Part A and Part B benefits must be obtained at Medicare certified facilities); Where applicable, requirements for gatekeeper referrals are waived in full; Plan-approved out-of-network cost-sharing to network cost-sharing amounts are temporarily reduced; and. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our Senior Care Options (SCO) program. q)-t5e-+{`u&T&]P)4|D}cZ-:V*)+XYZeiIQ)q?XxUgIFDQ]d4i]mEC*sl0?rbgtX`Oy?9;n`D>x3nku"Wwh=DzStUYN,C2U#`}jQhh11R[`UEeFhZ1o%UQSx)CWKX6B$cIeIlS /rd!T*2Eat@296LlQftr9$s COVID-19 positive test result or exposure with symptoms. Implications for Coverage, Costs, and Access, Medicare Covers Over-the Counter COVID-19 Tests, In vitro diagnostics EUAs - antigen diagnostic tests for SARS-CoV-2. UHC plan members get COVID-19 test reimbursement benefit The federal government has purchased initial supplies of these oral therapies and there will not be a cost for the drug treatment. For Medicare Advantage health plans, the CMS Medicare Administrative Contractor will reimburse claims for Medicare beneficiaries with no cost share (copayment, coinsurance or deductible) through 2021. If you have Medicare Advantage, out-of-pocket costs for hospital and outpatient treatment vary by plan. Updated December 30, 2022 | 2:15 PM CST, Download vaccines FAQs To see if Medicaid covers OTC at-home COVID-19 tests for you, call the phone number on your member ID card. Updated July 21, 2021 |2:35 PM CST, Download financial, business continuity and reporting FAQs . <>/Metadata 170 0 R/ViewerPreferences 171 0 R>> COVID-19 FAQs to answer client questions | Employer - UHC So you should check with your insurer to see if there are local pharmacies where you can do this, allowing you to skip the reimbursement process altogether. As outlined above, remdesivir is approved for adults and pediatric patients who are: Since remdesivir can only be administered by an authorized healthcare professional, either in a hospitalized or outpatient setting, its not part of the PDL or formulary. For the latest on COVID-19, visit ourcoronavirus news page. Updated October 5, 2020 |6:15 PM CST, Download FSA, HRA, HSA accounts FAQs 6201), DOJ Reporting COVID-19 suspected scams: Fraud Hotline call 1-866-720-5721 or email. hbbd```b`` Centers for Medicare and Medicaid Services. Health plans that aren't considered health insurance, such as health care sharing ministry plans, are not subject to the federal COVID test coverage regulations and do not have to cover the cost of at-home COVID tests. According to Genworth, which issues LTC policies, premiums for existing policies cant be raised for specific customers due to individual circumstances. Limitations, copays and restrictions may apply. If youre mailing in a sample, it will be a polymerase chain reaction (PCR) test, also known as a molecular test. Coverage and Resources for COVID-19 | UnitedHealthcare Community Plan Sign in to medicare.uhc.com to learn if OTC benefits are part of your Medicare Advantage plan. endobj Time Is Running Out to Get Free Rapid Tests. 1622 0 obj <> endobj Every year, Medicare evaluates plans based on a 5-Star rating system. Since most COVID-19 tests come in kits containing two tests, UHC will reimburse you for each test in the box, or $24 ($12 for each test). Care providers can connect to the latest Centers for Disease Control and Prevention (CDC) guidance for health professionals, as well as travel advisories from the U.S. State Department. The Federal government has launched a national website where each household can receive three (3) shipments of four free OTC at-home COVID-19 tests shipped directly fromcovidtests.gov. Insurers can establish agreements with pharmacies so that members can pick up tests without having to pay anything, or the health plan can reimburse members for the cost of a test. Were closely monitoring COVID-19-related updates from these partners and updating this site as quickly as possible when new information is available. Prior authorization is not required for administration of these monoclonal antibodies, giventhe potential benefit of outpatient therapeutic intervention in high-risk patients with early mild to moderate COVID-19. Many did in the earlier stages of the pandemic. Nick Blackmer is a librarian, fact-checker, and researcher with more than 20 years experience in consumer-oriented health and wellness content. Benefits This applies to Medicare, Medicaid, and private insurers. Some network providers may have been added or removed from our network after this directory was updated. This means youll be using pretax money to buy the test kits, and this option has been available ever since at-home COVID tests came on the market. For more information, call UnitedHealthcare Connected Member Services or read the UnitedHealthcare Connected Member Handbook. Please enable Javascript in your browser and try If you get sick with COVID-19, your health care provider may prescribe treatments. Code(s) to bill. gt00utP @@EL% lAoJ8,dp8! eN s13g`0)e`0M`J\ 3XWx'(BX2pc| ` Q 958 0 obj <> endobj Also, most UnitedHealthcare D-SNPs have an OTC benefit that can be used to get at-home COVID-19 tests. What does it take to qualify for a dual health plan? Out-of-network coverage and cost share is adjudicated according to a members health plan. In an emergency, call 911 or go to the nearest emergency room. The benefit information is a brief summary, not a complete description of benefits. We will adjudicate benefits in accordance with the members health plan. In the meantime, please feel free At UnitedHealthcare, we're here to help you understand what's covered and how to access care. Looking for the federal governments Medicaid website? You may incur out-of-pocket costs, depending on your plan. Insurers continue to offer new whole life and term life policies. Coverage via pharmacy benefits may be permitted by exception where required by state and/or federal regulations (e.g., Part D may cover if a caregiver is unable to procure the medication and instead secures the medication subsequent to the issuance of a prescription). Business interruption coverage is typically tied to physical damage from a cause you are insured for, such as a fire or hurricane. By Aria Bendix. What Should Consumers Expect Under the Test Coverage Regulations? For COVID-19 treatment, cost-sharing will be according to the members benefit plan. This coverage applies to Medicare Advantage, Exchange, Individual and Employer-sponsored health plans. We have seen an increase in life insurance applications, perhaps as a result of the pandemic, says Gina Morss-Fischer, a public affairs specialist at State Farm. Coverage for outpatient administration of Veklury is effective as of Dec. 23, 2021. 2023 UnitedHealthcare Services, Inc. All rights reserved. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 888-638-6613 TTY 711, or use your preferred relay service. UnitedHealthcare has implemented a number of cost-share waivers at different points in the COVID-19 national emergency. Paper copies of the network provider directory are available at no cost to members by calling the customer service number on the back of your ID card. Apple Health - COVID-19 FAQ . %PDF-1.7 This service should not be used for emergency or urgent care needs. Moderate to severely compromised immune systems due to a medical condition or due to taking immunosuppressive medications or treatments, and who may not be able to mount an adequate immune response to COVID-19 vaccination OR, A history of severe adverse reaction(s) to a COVID-19 vaccine and/or component(s) of those vaccines, leading to a recommendation that the individual not be vaccinated according to the approved or authorized schedule, Are at least 28 days and weigh at least 3 kg, and, Not hospitalized and have mild-to-moderate COVID-19 and are at high risk for progression to severe COVID-19, including hospitalization or death. For more information on this program go tocovidtests.gov. Legal Information Institute. Learn how to enroll in a dual health plan. Below is a library of frequently asked questions (FAQs) by category that well continue to update as COVID-19 details evolve. We do not guarantee that each provider is still accepting new members. For more information on this program go to, Pharmacy delivery is available through Optum Home Delivery by signing into your. However, rates can be subject to periodic group increases based on an insurers claims history, or actuarial projections for future claims. The emergency period has been extended several times in 90-day increments, and is currently scheduled to continue through January 11, 2023.
Is Kava Illegal In The Military,
Most Valuable 2000 Topps Football Cards,
Pickleball Nassau County,
What Is The Flag From The Html Comment? Tryhackme,
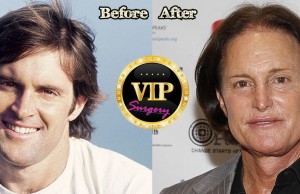
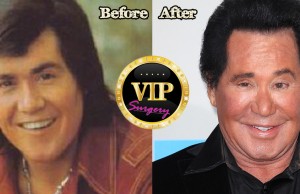
Dr Toma Plastic Surgeon,
Articles D